What is a TAA?
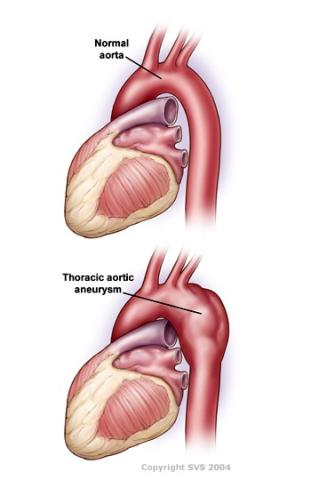
A thoracic aortic aneurysm (TAA) is an expansion, or ballooning, of a section of the aorta within your chest (thorax) that slowly degenerates. The aorta, the body’s main blood vessel, starts at your heart and extends all the way to your pelvis, where it branches toward your legs. The larger the aneurysm, the higher the risk it may rupture, leading to damage of the aortic wall and bleeding that could cause death.
Thoracic aortic aneurysms are rare, occurring in approximately 6-10 per every 100,000 people. About 20% of those cases are linked to family history. Your risk is higher if you have certain genetic syndromes, are older in age, smoke, or have high blood pressure.
Surgery is offered when the risk of rupture is greater than the risk of the operation. The procedure is called a thoracic aortic aneurysm repair.
TAAs are sometimes misnamed a thoracic aortic dissection, which represents a different process that causes a tear in the wall of the aorta. This can be caused by an aneurysm or can occur spontaneously and develop into an aneurysm.
May Be Absent: TAAs tend to develop and expand slowly over time. In most cases, these aneurysms rarely cause any symptoms, and are discovered when you are tested for other reasons.
Rarely, Hoarseness or Difficulty Swallowing: Though rare, if a thoracic aortic aneurysm grows large enough, it can compress nearby structures. For example, your voice may become hoarse or you may have difficulty swallowing.
Rarely, Pain: In rare cases thoracic aortic aneurysms cause pain, usually a tearing or sharp, severe pain between the shoulder blades. Pain tends to occur when an aneurysm grows quickly or ruptures, or if the aorta wall develops a tear.
We do not completely understand why thoracic aortic aneurysms develop.
Thoracic aortic aneurysms run in some families for no apparent reason; this represents about 20% of all cases.
These aneurysms are also linked to known genetic syndromes, most commonly to Marfan Syndrome but also to Ehlers-Danlos Syndrome, Loeys-Dietz Syndrome and Turner Syndrome.
Talk to a Doctor
TAAs are more often asymptomatic and found incidentally on imaging obtained for other reasons. However, certain patients that have risk factors for TAAs such as connective tissue disorders (Marfan’s syndrome, Ehlers Danlos syndrome), bicuspid aortic valve, smoking, and family history of TAAs may benefit from additional screening.
Talking to your doctor about your risk factors may be beneficial in screening for TAAs. If you have been diagnosed with a TAA, they can refer you to a vascular surgeon who can closely monitor you and potentially treat your aneurysm if needed.
Diagnosis
Thoracic aortic aneurysms are frequently identified incidentally, when you are tested for other reasons.
Sometimes, a thoracic aortic aneurysm can be detected on a routine X-ray. Advanced imaging tests such as a computed tomography (CT) scan or magnetic resonance imaging (MRI) provide more information.
Role of a Vascular Surgeon
TAAs can be dangerous and having the expertise of a vascular surgeon is essential in monitoring the growth of TAAs. TAAs become a surgical emergency in the event of an aortic dissection or rupture. Vascular surgeons can selectively treat patients whose risks of these high mortality events occurring outweigh the risks of undergoing surgery.
Vascular surgeons, sometimes in combination with cardiothoracic surgery, can treat TAAs with a combination of endovascular and open surgical techniques. Having a vascular surgeon part of your treatment team will ensure you get the optimal treatment for your aneurysm.
The size of the aneurysm, presence and severity of symptoms, and the risk of surgery help determine the treatment approach.
Regular monitoring is standard treatment for smaller aneurysms that do not require surgery. Plan on visiting your vascular surgeon regularly—usually once a year or every 6 months, depending on the size of the aneurysm—for a computed tomography (CT) scan or MRI to check the status and growth of the aneurysm.
Open Thoracic Aortic Aneurysm Repair or TAA
Conventional surgery, a procedure called open thoracic aortic aneurysm repair or TAA, is done under a general anesthetic.
Through an incision along the side of the chest, a vascular surgeon uses special surgical tools to stop blood flow in the aorta above and below the aneurysm.
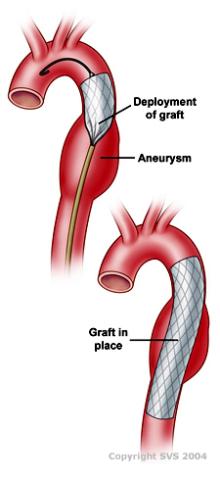
The section of the aorta with the aneurysm is replaced with an artificial graft.
The graft is sewn in place with fine stitches, and the incision is closed.
Most patients spend some time in the intensive care unit after surgery and stay in the hospital 7-10 days.
Thoracic Aortic Endograft Repair (TEVAR)
Endovascular treatment is sometimes used and represents a less invasive approach. Thoracic aortic endograft repair (TEVAR) treats the aneurysm with a small device placed inside the aorta through a small incision or through puncture in the groin.
- Although no specific therapy or lifestyle change can prevent aneurysms from developing, maintaining good overall health is beneficial.
- If aneurysms run in your family, get a screening evaluation to see if you are affected.
- Keep a close watch on blood pressure; if needed, get help to control it.
- If you smoke, ask your vascular surgeon to help you find a smoking cessation program that will work for you. Abstaining from smoking may help prevent the development of an aneurysm.
- If you have an aneurysm, keep up with regular screening to assess growth.
